Current Projects
In progress.
Our overarching goal is to understand the sexual and reproductive health (SRH) information needs of immigrant and newcomer youth in Canada to design an appealing and culturally appropriate app to that meets these needs. Anticipated outcomes of this project include: · To develop, implement, and evaluate of an innovative, user-centered mhealth intervention with immigrant adolescents that provide evidence-based information on SRH and ultimately improves adolescent SRH outcomes.
In progress.
Completed Projects
Summary: The Canadian Abortion Provider Survey (CAPS) 2019 is a CIHR funded study that examines characteristics of the Canadian abortion provider workforce, their quality of care and experience with stigma and harassment, particularly in relation to the 2017 introduction of mifepristone and publication of new SOGC clinical care guidelines. The specific aims of the survey are: Available from July to December 2020, we conducted a cross-sectional, self-administered survey of physicians, nurse practitioners, and administrators who provided abortion care in 2019. English and French surveys were available online, and recruitment materials were distributed through various health care organizations and networks. Our goal is to provide high-quality pan-Canadian survey data to inform abortion care planning for leaders of health policy, systems, services, and professional organizations in order to ensure and improve equitable high-quality abortion care in Canada. For more information, please click here. This survey is now closed. We are no longer recruiting participants. Acknowledgements: We would like to thank Canadian Institutes of Health Research (CIHR) for funding this study.
Summary: In July 2017, provincial nursing regulators instituted regulations to permit nurses to perform medical abortion, and in November 2017, Health Canada followed suit. Allowing Nurse Practitioners (NPs) to provide abortion services has the potential to address the current inequities in abortion services in Canada, particularly for rural and remote communities. National and provincial health policy regulators, system leaders, health professionals, and education experts have identified a priority knowledge gap: data is needed urgently to understand and address the needs of NPs initiating this new service in Canada. This study proposes to identify and address the factors necessary to ensure high quality, accessible provision of medical abortion services by Nurse Practitioners throughout Canada. For more information, please click here. This project has been awarded a three-year Canadian Institutes of Health Research (CIHR) Project Grant.
Summary: Although the gold standard for medical abortion care worldwide has been the use of mifepristone, a drug that terminates pregnancy, the medication was only recently approved in Canada in July 2015. The introduction of mifepristone presents an exceptional opportunity to better understand the effectiveness of health care provider training on adoption of medical abortion into practice and the impact on access to abortion, particularly for women in rural and remote areas. Our study of mifepristone implementation seeks to address the facilitators and barriers for successful initiation and ongoing provision of medical abortion service among health care professionals who have mifepristone certification, and how these relate to the distribution and availability of services throughout Canada. For more information, please click here
Summary: Access to abortion is inequitable in Canada. Most abortions are provided using surgery and are available only in large cities. Those living in rural and remote communities face particular difficulties to accessing abortion care. In 2017, Canada introduced mifepristone, a drug used for medical abortion. Because of Canada's unique mifepristone policies, this form of abortion could be available in primary care settings, which may improve abortion access in Canada through delivery closer- to-home. However, the actual impact of mifepristone introduction on abortion access, outcomes, and costs in Canada is not yet known. Also, countries around the world seek to understand the effects of Canada's unique deregulation of medical abortion. In this study, we will measure the impact of mifepristone introduction on abortion access, outcomes, and costs using Canada's comprehensive health administrative data. Research question: How has mifepristone medical abortion affected abortion access and service distribution, adverse event rates, and health system costs in Canada? Methods: This study uses linked population-based health administrative data to examine abortion outcomes, access, and costs for abortions before and after mifepristone introduction, in British Columbia and Ontario. Our team has conducted foundational mifepristone implementation research engaging health policy, system, service decision makers as well as health professionals. Federal and provincial health policymakers and system leaders are integrated into our research team to facilitate timely improvements. This study builds on our prior work which supports integrated knowledge translation of the results. Impact: This will be the first comprehensive examination of abortion services in Canada following mifepristone introduction, and will enable health policy, system and service delivery decision makers to further equitable access to safe, effective abortion care for patients across Canada and around the world.
Summary: Pregnancies following short interpregnancy intervals (conceived within 12 or 18 months of a prior delivery) are linked with increased risks of adverse pregnancy outcomes, including preterm birth, poor fetal growth leading to small-for-gestational age birth or low birthweight, and infant death. Current North American guidelines recommend that women wait a minimum of 18 months before becoming pregnant again, while the World Health Organization advises waiting at least 24 months. As preventing short interpregnancy intervals may be a strategy to reduce the burden of adverse fetal and infant outcomes, short interpregnancy intervals (<18 months) are monitored as a public health indicator in many countries across the globe, including the US. In this study, we will identify the optimal interpregnancy interval range for three high-risk obstetric populations that currently lack evidence to inform pregnancy spacing decisions. The findings of this study will inform pregnancy spacing recommendations to optimize healthy pregnancy and fetal and infant outcomes in these high-risk obstetric populations that most need targeted evidence to support pregnancy spacing decision-making. Read more here. Publications: Schummers L, Hutcheon JA, Norman WV, Liauw J, Bolatova T, Ahrens KA. Short interpregnancy interval and pregnancy outcomes: How important is the timing of confounding variable ascertainment? Paediatr Perinat Epidemiol. 2020;00:1–10. https://doi.org/10.1111/ ppe.12716 Schummers L. Interpregnancy interval and severe maternal morbidity – What can we learn from vital records data? Paediatr Perinat Epidemiol. 2020;34:388–391. https://doi.org/10.1111/ppe.12587
Summary: Early pregnancy loss (unintended pregnancy loss before 20 completed weeks of gestation) is a common adverse pregnancy outcome, with previous evidence reporting incidence ranging from 10% to 30% of detected pregnancies. The objective of this systematic review is to determine the incidence and range of early pregnancy loss in contemporary pregnant populations based on studies with good internal and external validity. Findings may be useful for clinical counseling in pre-conception and family planning settings, and for people who experience an early pregnancy loss. Click here to read more about the study protocol. Our comprehensive search strategy can be found here. Authors: Schummers L, Oveisi N, Hutcheon JA, Ahrens KA, Liauw J, Ohtsuka M, Norman WV
Summary: CART was awarded a CIHR Planning and Dissemination Grant in 2017 to support a planning meeting that aimed to develop a midwifery mifepristone implementation research study for Canada. In April 2018, CART, the Association of Ontario Midwives and the College of Midwives of Ontario hosted a Planning Meeting which engaged midwifery leaders from academic, regulatory, practice, health system and government settings to determine how best to design a study. From our planning meeting, it became clear that Canadian midwives are eager to ensure equitable and accessible care for prevention as well as management of unintended pregnancies. The CART MiPMaP Study: Midwifery Prevention and Management of Unintended Pregnancy (co-led by Drs. Wendy Norman and Liz Darling) will identify and address health policy, system and service barriers, facilitators and solution's to prompting the effective implementation and uptake of midwifery provision of contraception and abortion care. Proceedings from our April 2018 Planning Meeting: Acknowledgements: We would like to thank the Canadian Institutes of Health Research (CIHR) for funding our Planning Meeting.
Planning Canada's Midwifery Abortion Implementation Study
Summary: Our Canadian Sexual Health Survey pilot gathered information in 2014-15 regarding sexual and reproductive health, contraception use, pregnancy outcomes and accessibility of reproductive health services, enabling us to analyze how women plan and space their pregnancies. Unlike many countries, Canadian epidemiological data on sexual health to this date is very limited. Collection of this data is essential to inform health policies to improve the quality of life of Canadian women and their families. We hope that the government will be inspired to continue our project through the regular collection of nation-wide data about sexual health in the future, in order to create policies that are best representative of our Canadian population. To this end we evaluated the CSHS Pilot and created a proposed methodology and instrument for a national Canadian Sexual Health Survey. We are currently using the data obtained from our survey to create Canada's First Cost Effectiveness Model to predict, at a provincial level, the number of pregnancies and their subsequent outcomes based on survey indicators for sexual partners and activity, contraception use and social determinants of health. Policy analyses using this model can assist the government to evaluate the potential health and financial benefits of free contraception for women, thereby supporting evidence-informed policies for optimal health system strategies. Acknowledgements: We would like to thank the Canadian Institutes of Health Research (CIHR), the Michael Smith Foundation for Health Research and BC Women's Hospital for funding this study.
Summary: This BC Government-funded pilot program provides highly effective contraceptives free to all BC women at the time of abortion. This program was based on the recommendations that CART made to the Government, using data from two RCTs investigate post abortion contraception, linking participant data with government health administrative data to determine pregnancy outcomes. The Program preparations began mid-2016 and launched Jan 2017. CART is engaged in the evaluation of the program.
Summary: Women seeking an abortion often have difficult lives and face many obstacles to achieving their reproductive goals. For these and many additional reasons, they are at high risk for future unintended pregnancies. Despite the availability of intrauterine devices (IUDs), which offer very effective contraception, they are often uncommon in many marginalized populations. We hypothesize that more pregnancies will be prevented in women who undergo a second trimester abortion by inserting an IUD at the time of abortion, as opposed to scheduling a device placement later or choosing an alternate method of contraception. Our study uses contraception satisfaction questionnaire, clinical records and BC health databases to compare pregnancy rates with women using immediate and delayed IUDs after 2nd trimester abortions. We are also measuring secondary outcomes including comprehensive health economic analyses and device retention rates, complication rates and contraceptive method satisfaction. Immediate vs delayed insertion of intrauterine contraception after second trimester abortion: a Randomized Controlled Trial Acknowledgements: We would like to thank the Michael Smith Foundation for Health Research, the Canadian Institutes of Health Research (CIHR), the Child & Youth Health Research Network, and the Women's Health Research Institute for funding this study. 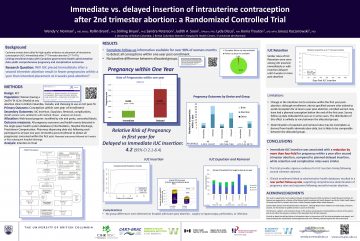
Norman WV, Brant R, Bryan S, Peterson S, Chen W, Soon JA, Dicus L, Trouton K, Kaczorowski J.
Summary: In this randomized controlled trial, consenting women choose to use an IUD after an abortion for a pregnancy of less than 12 weeks of gestation were randomized to device-type groups to receive immediate post-abortion placement of either a Flexi-T380(+) IUD, a device for which no current evidence on expulsion or effectiveness rates is available, or the Nova-T200 IUD, the only other brand of copper IUD available in Canada at the time of study initiation. The primary outcome measure is IUD expulsion rate at 1 year. Secondary outcomes include: pregnancy rate, method continuation rate, complication rates (infection, perforation), and satisfaction with contraceptive method. A non-intervention group of consenting women choosing a range of other post-abortion contraception methods, including no contraception, was included for comparison of secondary outcomes. Web-based contraception satisfaction questionnaires, clinical records, and government-linked health administrative databases will be used to assess primary and secondary outcomes.
Summary: We aim to develop and pilot-test a Canadian woman-centered contraception decision-making mobile application. This app will be “effectiveness-based” and will educate women about the efficacy of various contraceptive methods as well as important factors a women should consider when making decisions related to contraception. Acknowledgements: We would like to thank the Society of Family Planning and the Women's Health Research Institute for funding this study.
Summary: This study proposes a secondary analysis of the Canadian Community Health Survey (CCHS) data collected nationally by Statistics Canada and recently released. The World Health Organization (WHO) has classified contraceptives into four tiers of effectiveness. Since the CCHS collects data on contraception use among those under 24 years of age, we plan to determine correlates of contraceptive use, and particularly those for use of highly effective contraception and for the least effective methods of contraception, participants age 15 to 24 in Canada. Acknowledgements: We would like to thank the Women's Health Research Institute for funding this study.
Summary: There are numerous barriers and facilitators that affect women’s contraception choices. We are particularly interested in exploring contraception method choices and access among women on methadone or suboxone maintenance therapy for substance dependence. This unique patient group highlights the overlap of reproductive health and addictions medicine. Unfortunately, there is currently little Canadian data on this topic. This project utilizes the Canadian Sexual Health Survey (CSHS) as a tool to assess the barriers to care and knowledge that women experience. Acknowledgements: We would like to acknowledge the College of Family Physicians of Canada for funding this study through a grant from their Research and Education Foundation; the Children and Family Research Institute for provision of the RedCAP platform; and the UBC Faculty of Medicine for providing us with the opportunity to engage in clinical research.
Summary: Women in high resource nations are increasingly delaying childbearing until their thirties. Delayed childbearing poses challenges for the spacing of a woman’s pregnancies. Inter-pregnancy intervals greater than 12 months are associated with risk for adverse pregnancy outcome, yet increased maternal age at delivery is linked with higher risk. The optimal inter-pregnancy interval for older mothers is uncertain. This systematic review will aim to assess the relation between inter-pregnancy interval and perinatal and maternal health outcomes in women who delay childbearing to age 30 and older. Our review seeks to answer three questions: Acknowledgements: We would like to thank the Canadian Institutes of Health Research (CIHR) for funding this study through the CIHR-PHAC Chair in Family Planning Applied Public Health Research.
Summary: The goal of this research project is to perform a systematic review of the effectiveness of asking all reproductive-age women in primary care settings what their plans for pregnancy are. The evidence will be used to guide policy-making and future research to reduce unintended pregnancy and its many consequences. We will answer the following research question: “What are the effects of the incorporation of fertility intention questions in patients of reproductive age in primary care settings globally for pregnancy-related outcomes?”
Summary: We will determine timing discrepancies for hormonal contraceptive application approval between Health Canada (HC), the Food and Drug Administration (FDA) in the United States, and European Medicines Agency (EMA) and Medicines and Healthcare Products Regulatory Agency (MHRA) in the United Kingdom. The initial application dates and final approval dates for hormonal contraceptives approved between 2000 and January 2015 were obtained from HC, the FDA , EMA, and MHRA. In addition, hormonal contraceptives approved after 2000 by HC but before 2000 by the FDA, EMA, and MHRA were included. Generic versions of drugs were not included.
Summary: We will compare hysteroscopic tubal occlusion, one of the most commonly used permanent contraception methods; levonorgestrel releasing intrauterine contraceptive (LNG-IUC), a more effective method for prevention of pregnancy than tubal ligation but one that is often overlooked; and opportunistic salpingectomy, the removal of fallopian tubes. The latter has rapidly gained popularity in BC, cited for its theoretical prevention of ovarian cancer. It is important for women to be counselled on all available contraception options, however to date there exists no study that systematically brings together methods of permanent contraception. We hope to inform current policy guidelines by comparing the effectiveness, adverse effects, tolerability, non-contraceptive benefits and accessibility of these three contraceptive techniques.
Summary: During provincial surveys in 2011/12 on access to contraception in B.C carried out by our team, several Contraception Management (CM) certified nurses volunteered information on specific barriers and difficulties they had encountered in effectively delivering care. Many of those mentioned may be addressable at the system, regional or local level. To date, no comprehensive evidence exists on the effectiveness, facilitators and barriers for the CM certification practice. In order to assess if there are addressable issues to improve the effectiveness of the CM certification program, we propose an evaluation of the certificants’ experience in provision of this service. We hypothesize that addressable health system barriers may be preventing optimal effectiveness of the Nurse Contraception Management practice in British Columbia. Acknowledgements: We would like to thank the College of Family Physicians of Canada for funding this study.
